Abscesses are swollen areas of the body. They arise when the immune system perceives a foreign intrusion. They also result from internal phenomenon (such as a ruptured follicle) or external exposure to an organism (such as a bacteria or fungus) or foreign material (such as an injected drug or suture). There are abscesses that occur chronically (hidradenitis suppurativa) or acutely (a ruptured cyst).
A thorough personal history can help your doctor determine potential causes. People who have HIV or end-stage kidney disease are more likely to develop abscesses due to infections. A flea that burrows in the skin called Tunga penetrans may cause an abscess, so someone who has recently traveled may be at increased risk. Traveling or coming in contact with travelers is a risk factor for methicillin-resistant Staphylococcus aureus (MRSA). Does a family member have a similar lesion? MRSA can occur among family members.
Read on to find out more about abscesses.
- Furuncle/Carbuncle: A superficial infection of a hair follicle is folliculitis. When the infection encompasses the hair follicle and the surrounding tissue it is called a furuncle. A carbuncle is a larger lesion that includes several adjacent infected follicles. Community acquired MRSA has become increasingly more common and often presents as a furuncle with surrounding cellulitis. Treatment includes incision and drainage, culture for the organism, antibiotic therapy and a comparison of the antibiotic with the results of the culture once it is ready. About 10-20% of patients will develop recurrent furunculosis with ongoing abscesses.1
- Mycobacteria Furunculosis: Atypical mycobacteria (AMB) include but are not limited to Mycobacterium marinum, Mycobacterium fortuitum, and Mycobacterium chelonae. These organisms are found in soil, water, and decaying matter. Accidental breaks in the skin, surgery, pedicures and water promote risk for an AMB infection. One or more tender red nodules appear, then enlarge and contain pus. Biopsies are taken and sent for both histological and cultural evaluation. Minocycline typically can be initiated while awaiting results. Treatment may be required for months. The majority of cases of AMB resolve over the course of 6 months spontaneously without therapy. Treated cases naturally will respond more readily. Disseminated disease may occur in the immunocompromised.1
- Hidradenitis Suppurativa: This chronic inflammatory disease usually occurs in adolescence and consists of recurrent abscesses typically under the axilla and inguinal folds. Bacteria may or may not be found in the abscesses. Abscesses may rupture then either gradually resolve or progress into sinus tracts and scarring. Depending on the stage of the disease, cutting out the abscesses or scars may be necessary. An array of pharmacological interventions may be attempted first.1
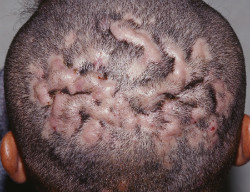
- Dissecting Cellulitis (DC) or Perifolliculitis Capitis Abscedens et Suffodiens: While poorly understood, occlusion of the hair follicle through hyperkeratosis (stacked skin) seems to initiate this disease. DC affects young men, particularly in ethnic groups. The vertex and posterior scalp are mostly affected. Pustules progress to deeper abscesses often causing sinus tracts, resulting in scarring and permanent loss of hair.1
Photos of a few abscesses
- Ruptured Epidermal Inclusion Cysts: Arising from the upper portion of the hair follicle, these cysts can rupture causing a foreign body reaction with subsequent inflammation, pus and pain. The foul smell is a result of a build-up of keratin within the cyst. Some cysts have such an intense reaction that the cyst wall is destroyed, thus eliminating the cyst altogether. Otherwise excision may be necessary to treat a persistent cyst.1
- Kerion: A kerion presents on the scalp as abscesses with inflammation and redness and may include pustular folliculitis, scale and erosions as a result of a fungal organism, mostly Trichophyton. Incidence of a kerion affects mainly children between 2-9 years of age. Multiple kerions can be present and in some individuals may be associated with fatigue, fever and enlarged lymph nodes. About 50% will recover normal hair growth after the infection has been treated and resolved. Permanent hair loss from the inflammatory response occurs in 25% of the population.1
- Tungiasis: This flea is native to the Caribbean region and West Indies, but has spread to Africa, India , Pakistan and Latin America. They prefer dry, warm sandy soil such as beaches or farmland. Due to increased travel, the disease is appearing in more countries. The infection is found primarily on the feet, often described as a white patch with a black dot. Pain and itching may accompany redness and swelling around the site. The flea burrows and usually dies within 2 weeks, but over the 1-2 weeks of feeding on the host’s blood, it will lay more than 100 eggs that fall to the ground through the central pore of the lesion. Wearing shoes in all areas can prevent this nuisance when traveling abroad. The abscess that often ensues sometimes must be surgically excised.2
Reference:
- Fitzpatrick JE, Whitney AH. Abscesses. In: Fitzpatrick JE, Whitney AH, Kyle, WL, eds. Urgent care dermatology: symptom-based diagnosis. Canada: Elsevier; 2018: 217-228.
- Ngan V. Tungiasis. DermNet New Zealand: All About the Skin website. https://www.dermnetnz.org/topics/tungiasis/. Updated 2008. Accessed November 14, 2017.